In part one of my post on meniscus tears, I discussed the role of the meniscus in knee function, ways it can be injured, symptoms of a tear, and tests and exams a physician can use to diagnose them. Once that is established, the discussion quickly turns to how best treat these tears.
The most important thing I emphasize with patients is that every meniscus tear is different. There are many things to consider when discussing the best treatment option. The location and type of tear, the patient’s age and activity level, associated symptoms such as if the knee is locking or not, and the presence of other conditions such as osteoarthritis and ligament tears are all important considerations in choosing the best way to proceed
Nonoperative Options
The broadest way to break down treatment options is whether the tear will be treated with or without surgery. With this in mind, there are several instances where most patients will be recommended to not consider nonoperative options. If the knee is locked because of certain meniscus tears, nonoperative treatment is unlikely to lead to successful results. Worst still, the locked fragment can damage the articular surface of the joint if left for too long. Further, meniscus tears associated with significant ligament injuries such as ACL, or anterior cruciate ligament, in athletes or those requiring full stability of their knee will often have their meniscus tear treated surgically at the same time as their ligament tear.
So, for those tears not meeting those criteria, what can be done to hopefully avoid a trip to the operating room? Conservative options abound for many types of meniscus tears, especially smaller degenerative type tears associated with arthritis. Rest, ice, anti-inflammatory medication, and physical therapy can decrease the pain and swelling associated with these tears. Corticosteroid injections have been utilized for years and can be effective if these first line treatments fail to relieve your pain. Newer medications and treatments, such as viscosupplementation and PRP, or platelet rich plasma, are not as well studied but are being increasingly used in the conservative management of certain types of meniscus tears. Each of these can be performed in the physician office with minimal down time. I’ve found nonoperative approaches to be most successful in patients who have few mechanical complaints, that it catching or locking of the knee, or a sensation of popping with activities.
Operative Options
For patients who have failed conservative approaches or have more significant symptoms, surgery can offer relief that can allow you to return to the activities that sports, your job, and life demand. Meniscus tears are now treated almost exclusively via arthroscopic surgery. This surgery utilizes small incisions and instruments the size of a pencil and smaller to assess the tear and manage it.
During surgery, meniscus tears can be addressed one of two ways. The tissue will either be sewed back together, or repaired, or more commonly, trimmed out to remove the damaged tissue that is causing pain. Meniscus repairs are much less common because there are few tears that meet the criteria for this type of treatment. Factors such as your age, the type and location of the tear, the quality of the tissue, and the presence of arthritis are all factors your physician should discuss as before surgery. The final determination of whether the meniscus can be repaired or not will occur during surgery. If it can be repaired, a variety of options exist. Suture can be placed into the meniscus through the same arthroscopic incisions, or through needles placed through the skin. Some tears are better treated by making incisions on the side of the knee to more safely and securely pass the sutures. Meniscus repair requires prolonged rehabilitation, often with crutches, bracing, and periods of nonweightbearing and physical therapy to allow the meniscus to heal.
The more common approach of trimming out the damaged tissue, or partial meniscectomy, does not require the same precautions as a meniscus repair, yet still requires a period of rest and often physical therapy to allow a full recovery. Crutches or a cane can allow the knee to rest for a short period of time after surgery, and limiting how much walking and other activities one does will minimize swelling that can slow down the rehabilitation process
Recognizing that a variety of options exist in treating your meniscus tear is the first step in obtaining a successful outcome. A range of treatments can typically be offered and the first step does not always have to be surgery. If surgery is chosen, most patients will reach a full recovery and have the chance to return to all levels of previous activity. Talk to your physician about your individual case and find what works for you.
Tuesday, February 12, 2013
Tuesday, February 5, 2013
Meniscus Tears Part One
The human knee joint can take a tremendous toll in the course of athletic participation, with injury, even everyday activities. A force of three to six times one’s body weight is transmitted through the knee every step one takes. To spread that load and lessen damage to the joint, we rely on a structure called the meniscus, semicircular bands of tissue spanning each side of the joint which service to distribute load and stabilize the knee.
Meniscus tears can occur in a variety of settings. Athletic injury, work accidents, and even minor trauma to the knee can cause acute tears. Age related changes often result in chronic or degenerative tears, of the meniscus which can commonly be seen in the setting of osteoarthritis.
Typical symptoms of a meniscus tear include pain, swelling, and sometimes a sensation of a pop when it occurs. Other associated symptoms can include locking or catching of the knee, a feeling of giving way, and a loss of range of motion
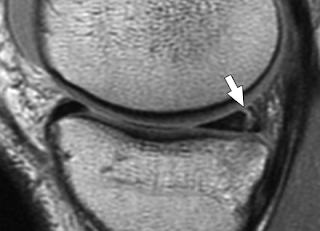
When these symptoms are present, a thorough physical examination is the first step for you and your physician. X-rays can be helpful to evaluate for other conditions such as a fracture, or more commonly osteoarthritis. Magnetic resonance imaging, or an MRI, can fully evaluate the soft tissues of the knee including the meniscus.
Meniscus tears can occur in a variety of settings. Athletic injury, work accidents, and even minor trauma to the knee can cause acute tears. Age related changes often result in chronic or degenerative tears, of the meniscus which can commonly be seen in the setting of osteoarthritis.
Typical symptoms of a meniscus tear include pain, swelling, and sometimes a sensation of a pop when it occurs. Other associated symptoms can include locking or catching of the knee, a feeling of giving way, and a loss of range of motion
When these symptoms are present, a thorough physical examination is the first step for you and your physician. X-rays can be helpful to evaluate for other conditions such as a fracture, or more commonly osteoarthritis. Magnetic resonance imaging, or an MRI, can fully evaluate the soft tissues of the knee including the meniscus.
Subscribe to:
Posts (Atom)